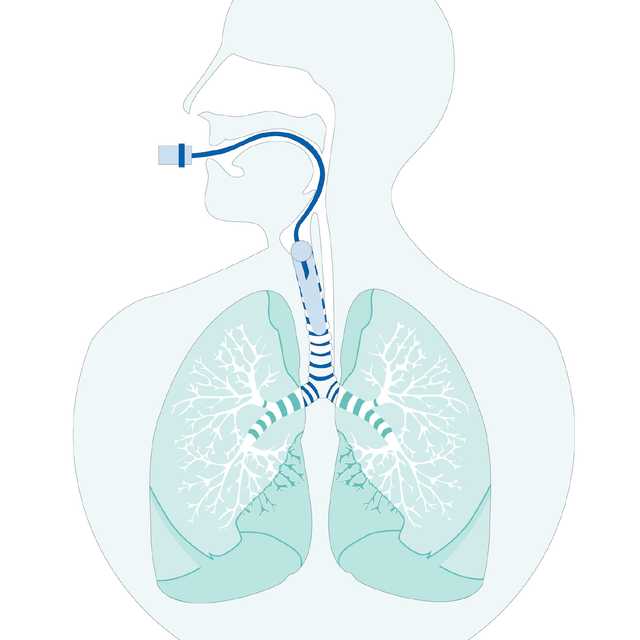
Continuously optimized and controlled cuff pressure supports ventilation therapy and protects your patients from ventilator associated pneumonia (VAP) and tracheal injuries (
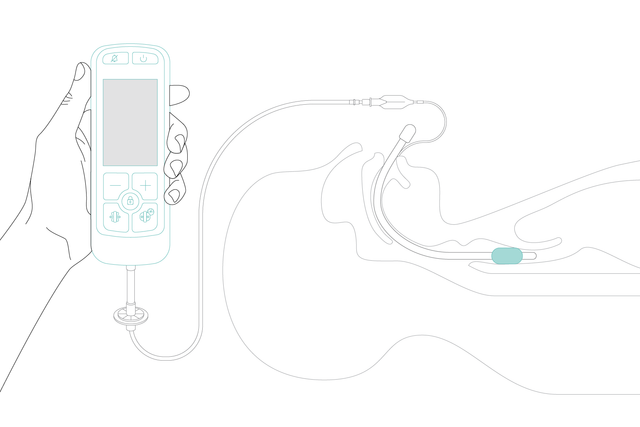
With IntelliCuff, most of this work is done for you. Simply set the desired cuff pressure and IntelliCuff maintains it automatically. The device can operate within a wide, but safe range of pressures for various cuffed endotracheal tubes.
Whether you use it for air transport with quickly changing ambient pressure or in the operating room during N2O narcosis or surgery, IntelliCuff continuously monitors and maintains optimal cuff pressure for greater patient safety. Even during some of the most critical situations (


Suitable for adults, pediatrics and neonates. IntelliCuff secures airway management in a range of different situations ‑ in the ICU and the operating room, or during transport. You can use it for emergency rescue on land or in the air ‑ even at higher altitudes.

We use IntelliCuff as a standard feature to help prevent VAP in mechanically ventilated patients. IntelliCuff controls the cuff pressure automatically and regularly. This is a great help for us caregivers since we don’t have to check the cuff pressure manually every hour.
Head of ICU Nursing Department
Grisons Cantonal Hospital, Chur, Switzerland




Different interfaces allow you to mount the IntelliCuff wherever you need it. With just one click.


The IntelliCuff standalone device is the perfect companion for Hamilton Medical ventilators.