作者: Jean-Michel Arnal,高级医师,Ste Musse 医院,Toulon,法国
日期: 23.04.2019
PEEP 用于保持肺通气,防止呼气末肺塌陷。然而,PEEP 可能使正常通气的肺过度扩张,并损害肺灌注。因此,PEEP 的任何变化都可能以不可预测的方式影响整体通气/灌注比值。
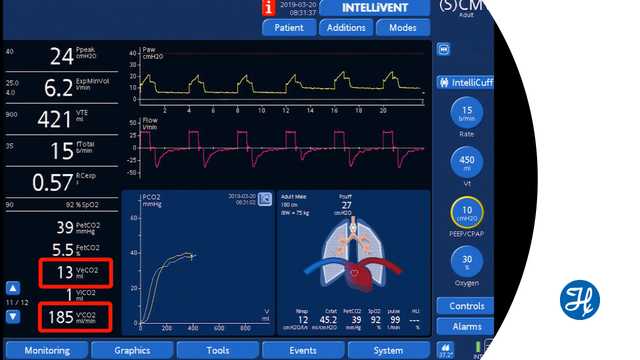
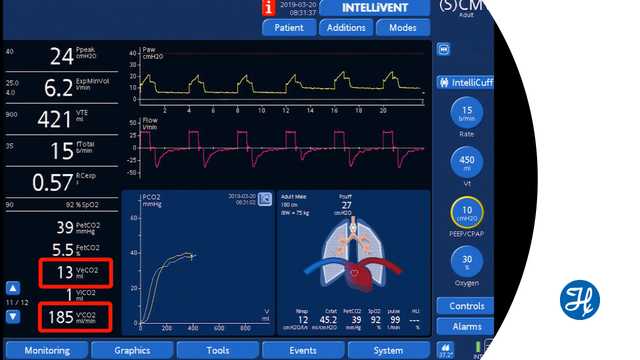
容积二氧化碳图测量每次呼吸呼出的二氧化碳容量 (VeCO2)。PEEP 发生变化后,假设心血管功能和潮气量稳定,VeCO2 的增加意味着整体通气/灌注比值有所改善。相反,VeCO2 的减少意味着通气/灌注比值正在恶化。VeCO2 变化迅速,几分钟后恢复到基线。
这种方法的局限性在于临床医生监测通气/灌注比值的快速变化,例如由于肺过度扩张和肺灌注损伤或改善引起的变化。
PEEP 改变后,肺复张或肺塌陷可能需要更长的时间,并且无法通过该方法进行评估。
观看下面的视频,观看使用 Hamilton Medical 哈美顿医疗公司呼吸机进行通气的演示。
完整引文如下: (
学习如何解读容积二氧化碳图及了解容积二氧化碳图的优点和临床应用。包括自测内容!