作者: Hamilton Medical 哈美顿医疗公司
日期: 11.09.2017
Last change: 28.07.2023
Transpulmonary pressure measurement changed to monitoring病人进行机械通气时的最大挑战之一是找到呼气末正压 (PEEP) 的正确设置。通过使用跨肺压监测来区分肺压和胸壁分压,这项任务可以变得更容易。
能够区分肺压和胸壁分压有助于设置最佳 PEEP,定义安全的驱动压力和平台压范围,以及滴定和优化肺复张操作。但当在气道开口处测量的压力无法用于准确评估施加于肺部的应力和张力时,如何能够区分他们呢?区分他们的一个简单方法是通过使用食道压测量。气道压力减去吸气末或呼气末闭塞期间测量的食道压,即为跨肺压,其代表肺部的真实扩张压力。
跨肺压监测在 HAMILTON-G5/S1(
在急性呼吸窘迫综合征 (ARDS) 病人中,可以设置 PEEP,从而在呼气末达到 0 至 5 cmH2O 的跨肺压,目的是防止远端气道和肺泡反复打开和关闭引起的不张性肺损伤。跨肺压监测也可用于设置 ARDS 病人的潮气量和吸气压力,并与 P/V Tool® 一起评估肺的可复张性和进行肺复张操作。
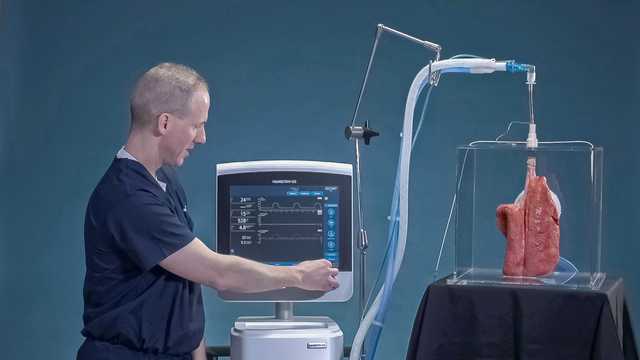
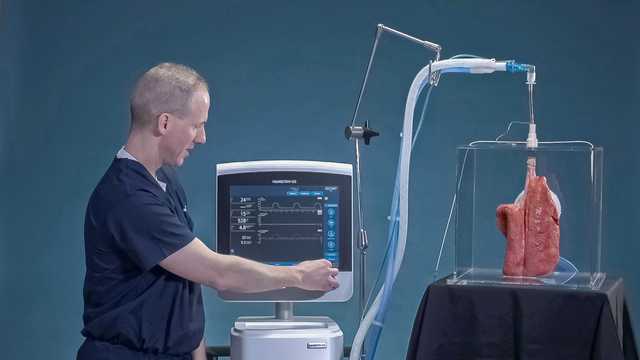
下面的视频向您展示了如何在 HAMILTON-G5 呼吸机上使用跨肺压监测设置 PEEP。

跨肺压监测可优化 PEEP、潮气量和吸气压力(